North Carolina Man Declared Brain Dead: Shocking Hospital Update!
The Shocking Case of a North Carolina man Declared Brain dead
In a gripping story that has left many questioning the ethics and accuracy of medical practices, a North Carolina man was declared brain dead, only to later exhibit signs of life. This incident sparked widespread media attention and raised crucial discussions surrounding organ donation protocols and the definition of brain death.
The Initial Declaration of Brain Death
The incident began with the unfortunate news of a man in North Carolina being declared brain dead. As per the medical team’s assessment, the man was deemed clinically dead, leading his family, particularly his wife, to begin planning his funeral. The declarations surrounding brain death are serious and often irreversible, which is why the family’s grief was compounded by the finality of this declaration.
A Turn of Events
However, in a startling twist, the hospital later contacted the man’s wife with shocking news: he had shown signs of movement and responsiveness to stimuli. This revelation contradicted the previous determination of brain death, leading to a whirlwind of emotions for the family who was already in the process of mourning. The man’s unexpected reactions raised numerous questions about the reliability of brain death diagnoses and the procedures that follow.
The Ethics of Organ Donation
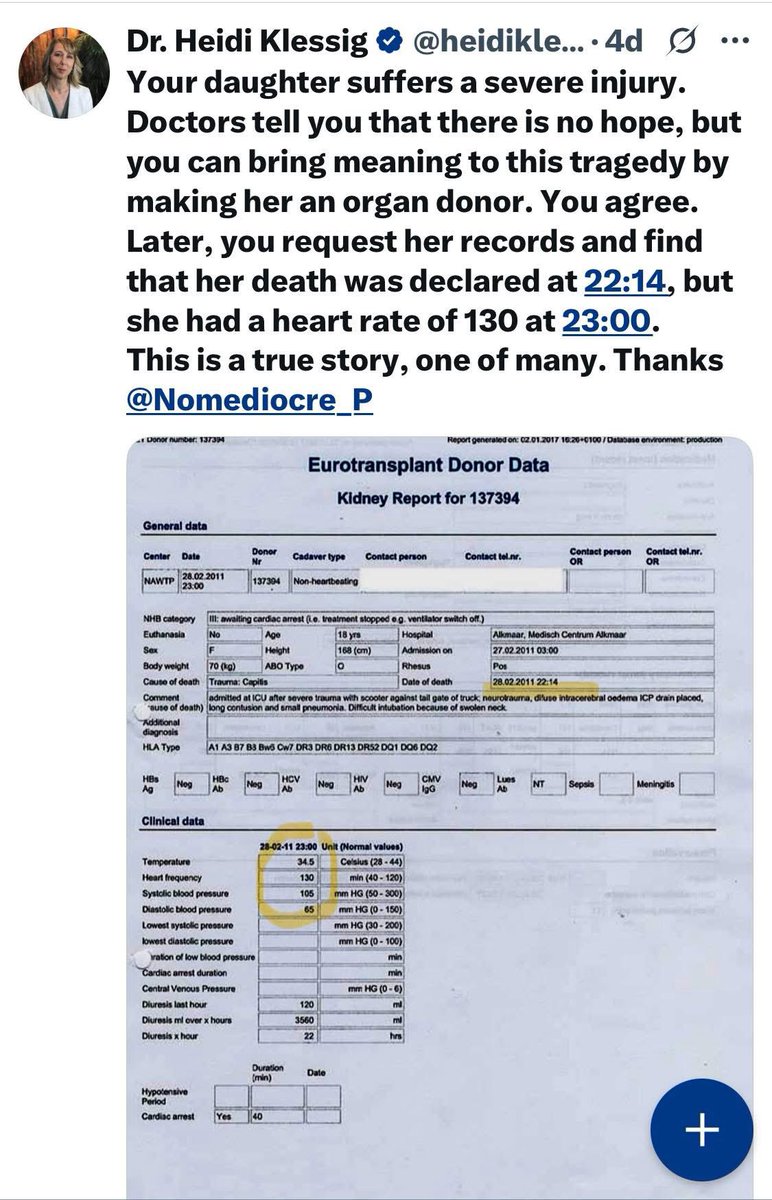
This case has ignited debates about the ethics involved in organ donation, especially when the determination of brain death is made. The notion of declaring someone brain dead is critical for organ donation processes, as it allows for the procurement of organs for transplantation. However, this incident raises significant concerns about how medical professionals determine brain death and the potential for human error in such critical assessments.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
Defining Brain Death
Brain death is defined as the irreversible loss of all functions of the brain, including the brain stem. It is distinct from a coma or vegetative state, where some brain functions may still be present. However, the criteria for determining brain death can sometimes be complex and may vary from one medical facility to another. This inconsistency in protocols can lead to life-altering consequences, as seen in this case.
The Role of Medical Professionals
Medical professionals are tasked with making life-and-death decisions based on their expertise and available technology. However, as this North Carolina case demonstrates, there can be discrepancies in diagnosis. The reliance on technology and medical assessments underscores the necessity for rigorous protocols and checks before declaring brain death, as these decisions are often irreversible.
The Impact on Families
For families, the emotional toll of such cases can be profound. The sudden shift in circumstances can lead to confusion, anger, and a plethora of emotions. Families may feel betrayed by the medical system they trusted, and the psychological ramifications of losing a loved one only to discover that they might still be alive can be devastating.
A Call for Change
In light of this incident, there is a growing call for changes in how brain death is diagnosed. Advocates argue for more stringent evaluation processes, including the use of advanced imaging techniques and multidisciplinary approaches to confirm brain death. These changes could help prevent future occurrences of misdiagnosis and ensure that families do not have to endure such heart-wrenching experiences.
Public Awareness and Advocacy
This case has sparked conversations not only among medical professionals but also within the general public. Awareness about the nuances of brain death and organ donation is critical. Many individuals may not fully understand what it means to be declared brain dead, nor the implications it has for organ donation. Public discourse surrounding this topic can lead to better-informed decisions regarding organ donation and the treatment of brain-dead patients.
The Importance of Informed Consent
Informed consent is a crucial component of medical ethics, particularly in organ donation. Families should be fully educated about the processes involved and the implications of a brain death diagnosis. This incident highlights the need for transparency in medical communications and the importance of ensuring that families understand their options and the circumstances surrounding their loved ones’ health.
Conclusion
The shocking case of the North Carolina man who was initially declared brain dead but later showed signs of life serves as a poignant reminder of the complexities involved in medical diagnoses and the ethical considerations surrounding organ donation. It emphasizes the need for rigorous protocols and transparency within the medical community to prevent future tragic errors.
As discussions continue about the implications of this case, it is vital for both medical professionals and the public to engage in meaningful conversations about brain death and organ donation. Educating ourselves on these topics can help ensure that families are supported and informed during some of the most challenging times of their lives.
In summary, this incident not only highlights the need for improved medical practices but also underscores the importance of compassion and understanding in the face of life-altering decisions. As we move forward, the lessons learned from this case could pave the way for better protocols that prioritize patient dignity and family support.

“They did this to the North Carolina man who made the news after he was declared brain dead as an organ donor.
His wife went home to plan his funeral and the hospital called and told her he had moved and reacted to stimuli and was not brain dead.
But, they said it doesn’t… pic.twitter.com/ySuAoQA3o6
— “Sudden And Unexpected” (@toobaffled) June 4, 2025
They did this to the North Carolina man who made the news after he was declared brain dead as an organ donor.
Picture this: a North Carolina man, full of life, suddenly finds himself in a terrifying situation where he’s declared brain dead. His family is left grappling with the shock, trying to come to terms with their loss. This scenario, unfortunately, isn’t just a plotline from a medical drama but a real-life story that unfolded recently, shocking many and raising critical ethical questions about organ donation and medical practices.
His wife went home to plan his funeral and the hospital called and told her he had moved and reacted to stimuli and was not brain dead.
Imagine the gut-wrenching moment when his wife, heartbroken and in despair, begins the painful process of planning a funeral. In the midst of these tragic preparations, she receives a call from the hospital that flips her world upside down. The doctors inform her that her husband had shown signs of movement and responsiveness, indicating that he was not, in fact, brain dead. Can you fathom the emotional rollercoaster she must have experienced, swinging from the depths of grief to a flicker of hope? This twist of events not only highlights the complexity of brain death diagnoses but also raises serious concerns about the protocols followed in organ donation cases.
But, they said it doesn’t…
Now, here’s where things get even more complicated. Despite the miraculous signs of life, the hospital’s stance on the situation left the family and many others questioning the ethics of organ donation practices. The phrase “But, they said it doesn’t…” echoes the frustration felt by countless families who fear that their loved ones may be prematurely declared brain dead. This incident has sparked widespread discussions about the criteria used to declare brain death and the potential for human error in such critical situations.
The Importance of Accurate Brain Death Determination
Determining brain death isn’t as straightforward as it seems. Medical professionals must conduct a series of tests to confirm that there is no brain activity. This includes examining reflexes, responses to stimuli, and various neurological evaluations. However, the inconsistency in these assessments can lead to devastating consequences for families. It’s crucial for hospitals to adhere to strict guidelines and ensure that every possible measure is taken to confirm brain death before proceeding with organ donation.
Ethical Concerns Surrounding Organ Donation
The ethical implications of declaring someone brain dead are huge. Families often find themselves in a vulnerable state, forced to make life-altering decisions under duress. The North Carolina man’s case underscores the need for transparency in the organ donation process. Families should be fully informed about the criteria for brain death and the potential for error in these assessments. It’s not just about saving lives through organ donation; it’s about ensuring that the rights of the living are respected and upheld.
Public Perception of Brain Death and Organ Donation
Public perception plays a significant role in the organ donation process. Many individuals are hesitant to agree to organ donation due to fears about how brain death is determined. The North Carolina man’s story can lead to increased skepticism and mistrust towards healthcare systems. It’s essential for hospitals and medical professionals to engage in open dialogues with the community to address these fears and foster trust. Education and awareness campaigns can help bridge the gap between medical practices and public understanding, allowing for a more informed decision-making process.
The Role of Advocacy Groups
Advocacy groups are stepping up to support families navigating the organ donation process. These organizations aim to provide resources, education, and emotional support to those facing difficult decisions. They advocate for ethical practices and push for reforms in how brain death is determined. By amplifying voices like the North Carolina man’s family, these groups work to ensure that no one else has to endure the same trauma. Their efforts are crucial in promoting change within the healthcare system, ultimately leading to better outcomes for patients and their families.
What Can Be Done to Prevent Future Incidents?
To prevent tragic incidents like the North Carolina man’s, it is essential that healthcare institutions strengthen their protocols surrounding brain death assessments. This includes regular training for medical staff, implementing consistent testing procedures, and engaging in peer reviews of cases where brain death is declared. Additionally, hospitals should provide families with clear information about the process and encourage them to ask questions. Empowering families with knowledge can help alleviate fears and enhance trust in the medical system.
The Importance of Communication
Effective communication between healthcare providers and families can make a world of difference. Families should feel comfortable expressing their concerns and asking for clarification about complex medical terms and processes. Hospitals need to create an environment where open dialogue is encouraged, allowing families to voice their fears and anxieties. This approach can lead to better understanding and can help foster a more supportive atmosphere during incredibly challenging times.
Moving Forward: A Call for Change
The North Carolina man’s story is a stark reminder of the complexities surrounding brain death and organ donation. It highlights the urgent need for reforms in how these processes are handled. By advocating for better practices, improved communication, and increased transparency, we can work towards ensuring that no family has to face the agony of questioning the circumstances surrounding their loved one’s death.
Conclusion: Learning from Tragedy
While this tragic story is one of heartbreak, it can also be a catalyst for change. By learning from these incidents, we can strive to create a healthcare system that respects the dignity of all individuals, ensuring that organ donation processes are conducted ethically and compassionately. It’s essential that we honor the lives lost by advocating for a system that prioritizes the rights and well-being of families during their most vulnerable moments.
“`
This article delves into the complex issues surrounding brain death and organ donation, using a real-life case to illustrate the emotional and ethical challenges involved. It emphasizes the importance of accurate diagnoses, ethical practices, and open communication to foster trust between patients, families, and healthcare providers.