Shocking Revelation: Nebraska Boy’s Body Kept “Alive” for 20 Years!
The Controversial Case of a Nebraska Boy: Brain death and Long-Term Research
In a shocking and ethically complex case from 1983, a four-year-old boy from Nebraska was declared brain dead following a tragic incident. The implications of this case have resonated through the medical community and society at large, prompting discussions about medical ethics, life support, and the treatment of brain-dead individuals. This summary delves into the key aspects surrounding this case, the ethical considerations, and the ongoing debates it has sparked.
Background of the Case
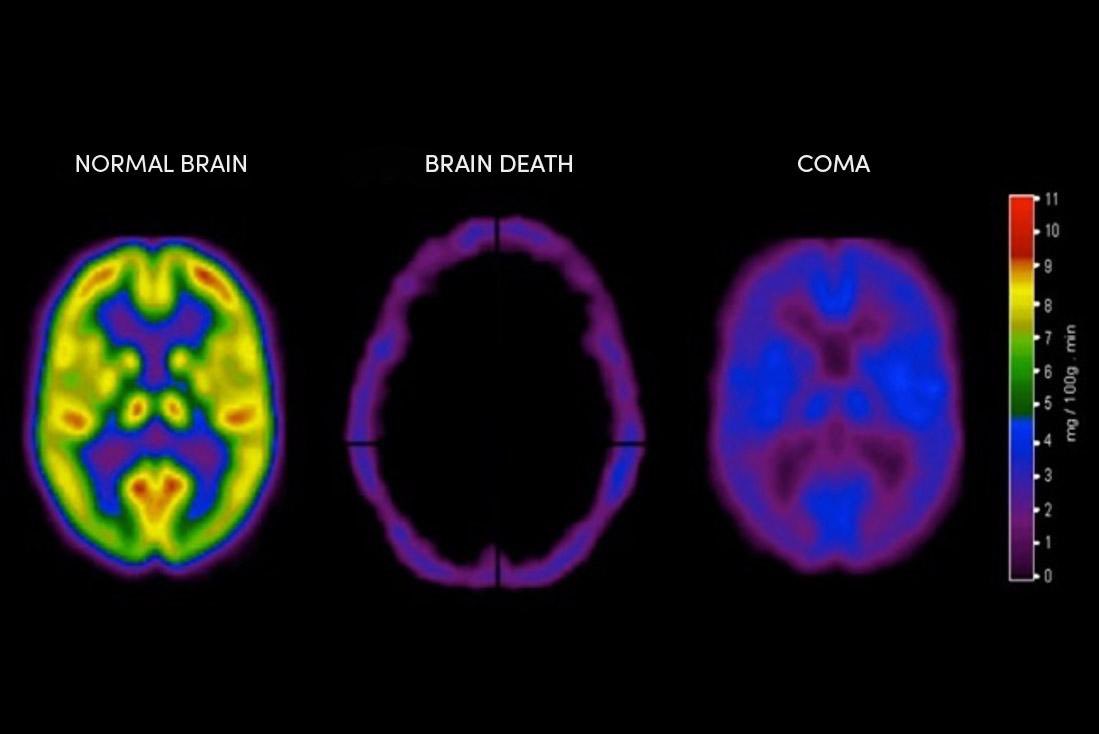
The case began in 1983 when a four-year-old boy suffered a severe medical event that ultimately led to his declaration of brain death by a team of medical professionals. Brain death is defined as the irreversible loss of all functions of the brain, including the brainstem. This condition is legally and medically recognized as death. However, in a controversial decision, doctors opted to maintain the boy’s body on life support for over two decades, ostensibly for research purposes.
Ethical Implications of Long-Term Life Support
The decision to keep a brain-dead individual on life support raises profound ethical questions. Many in the medical community argue that brain death should be treated as a definitive endpoint. Keeping a body "alive" without consciousness or potential for recovery challenges the very definition of life and death.
One of the critical ethical concerns is the potential for exploitation. Critics argue that maintaining the boy’s body for research purposes could be viewed as a violation of his dignity and autonomy. When a patient is declared brain dead, the ethical justification for using their body for research must be weighed carefully against respect for the individual and the rights of their family.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
The Medical and Scientific Perspective
From a medical standpoint, the extended use of the boy’s body for research could have provided valuable insights into neurological conditions and the implications of brain death. Research in this area can contribute to advancements in medical science, particularly in understanding brain injuries and developing new treatment modalities. However, it is essential to balance these potential benefits with the ethical responsibilities owed to the deceased and their family.
Public Reaction and Media Coverage
The case garnered significant media attention and public outcry, with many questioning the morality of the doctors’ decision. The narrative surrounding the boy’s prolonged life support became a focal point for discussions about end-of-life care, medical ethics, and the rights of patients and their families. Social media platforms, including Twitter, became avenues for sharing opinions and information about the case, further fueling public interest and debate.
Legal Considerations
In addition to ethical implications, the case also raises legal questions about the rights of families and the definition of death. Laws governing brain death can vary significantly by jurisdiction, and the decision to maintain life support in such cases can be influenced by legal, familial, and cultural factors. The Nebraska case underscores the need for clear legal frameworks that protect the rights of individuals and their families in end-of-life situations.
The Role of Families in Decision-Making
Families play a crucial role in end-of-life decisions, particularly in cases involving brain death. The emotional weight of these decisions can be overwhelming, and families often find themselves navigating a complex landscape of medical information, ethical considerations, and personal beliefs. In the Nebraska case, the family’s perspective and their wishes regarding the continuation of life support were likely significant factors in the doctors’ decision-making process.
The Impact on Future Medical Practices
The Nebraska case has influenced discussions about medical practices surrounding brain death and life support. It has prompted healthcare professionals to reevaluate the criteria for brain death and the protocols for maintaining life support in similar cases. The case serves as a reminder of the importance of transparent communication between medical teams and families, as well as the need for comprehensive guidelines that address the ethical complexities of such situations.
Conclusion: A Legacy of Controversy
The story of the four-year-old boy from Nebraska remains a poignant and controversial chapter in the discourse surrounding brain death and medical ethics. As advancements in medicine continue to evolve, the lessons learned from this case will likely inform future practices and policies regarding end-of-life care. The ethical implications, legal considerations, and emotional ramifications of maintaining a brain-dead individual on life support will continue to be subjects of intense discussion and reflection within the medical community and society.
By examining such cases critically, we can foster a more compassionate and ethically sound approach to medical practice, ultimately ensuring that the dignity and rights of individuals, even in death, are upheld. As we move forward, it is essential to engage in ongoing dialogue about these sensitive issues, learning from past experiences to create a more informed and empathetic healthcare system.
Keywords for SEO Optimization
- Brain death
- Life support
- Medical ethics
- End-of-life care
- Nebraska case
- Ethical implications
- Family decision-making
- Neurological research
- Medical practices
- Life support ethics
This summary provides an overview of the complex issues surrounding the case of the Nebraska boy, highlighting the ethical, medical, and legal considerations that continue to resonate within the healthcare community.

After a 4 year old from Nebraska was declared brain dead in 1983, doctors kept his body “alive” for more than 20 years for research. pic.twitter.com/U7ORGKSxSj
— Morbid Knowledge (@Morbidful) May 25, 2025
After a 4 year old from Nebraska was declared brain dead in 1983, doctors kept his body “alive” for more than 20 years for research
When we think about the world of medical research, it often conjures images of cutting-edge technology, groundbreaking treatments, and scientific breakthroughs. However, there are instances in medical history that leave us with more questions than answers, particularly when ethical lines are blurred. One such case involves a tragic story from Nebraska in the early 1980s, where a four-year-old child was declared brain dead but remained in a sort of limbo for over two decades. This story invites us to explore the ethical implications of medical research, the boundaries of human dignity, and the societal responsibilities we have toward the deceased.
The Initial Tragedy
Imagine a vibrant four-year-old boy, filled with curiosity and life, suddenly facing a devastating fate. In 1983, this young child from Nebraska suffered a catastrophic event that led to his brain death. His family was faced with an unimaginable loss, and the medical community was confronted with a heartbreaking decision. Declaring someone brain dead is a complex process that involves multiple tests and assessments to ensure that brain function has irreversibly ceased. In this case, the doctors determined that the child had met all criteria for brain death, and thus, life support was disconnected.
For the family, this was a moment of profound sadness. But what unfolded next was something that would not only change their lives but also leave an indelible mark on medical ethics.
The Controversial Decision
Following the declaration of brain death, doctors made a controversial choice: they decided to keep the child’s body “alive” for research purposes. This decision raises critical questions about medical ethics and the sanctity of the human body. The rationale given for this choice was the potential for scientific advancement. Researchers believed that studying the child’s brain and bodily functions could yield insights into pediatric care and neurological conditions. This practice of keeping a brain-dead body on life support is not common, but it has occurred in certain instances where the medical community feels that valuable research could be gained.
For over 20 years, the child’s body was maintained in a state that many would argue should not exist. The ethical implications of this decision are staggering. How do we balance the pursuit of knowledge with the respect and dignity afforded to every human being, even after death?
The Implications of Extended Research
Keeping a body “alive” for research purposes raises a myriad of ethical and moral dilemmas that are difficult to navigate. For instance, what rights do the deceased—and their families—hold regarding how their bodies are treated after death? In many cultures, the body is sacred, and there are established rituals that honor the deceased. The decision to prolong life support for research can be seen as a violation of these principles.
Moreover, this case brings up questions about consent. Did the family consent to this arrangement? Were they fully informed about what it meant to keep their child’s body in a state of suspended animation for research? These questions highlight the need for clear guidelines and ethical standards in medical research, particularly when it involves vulnerable populations, such as children.
Medical Research and Ethics
This case has become a touchstone for discussions about medical ethics, particularly in research involving human subjects. The principles of autonomy, beneficence, non-maleficence, and justice must guide any research involving human bodies. In this situation, the line between beneficence (doing good) and non-maleficence (avoiding harm) is particularly blurred.
The concept of autonomy is also crucial. In medical ethics, patients (or their families) should have the right to make informed decisions about their treatment and care, even after death. The lack of clear communication and consent in this case raises concerns about whether the family’s wishes were genuinely respected.
Furthermore, this case invites us to examine the broader implications of medical research. While advancements in medicine can save lives and improve healthcare, they must be pursued with a commitment to ethical standards. The legacy of this young child’s situation serves as a reminder that the pursuit of knowledge should not come at the expense of human dignity.
The Legacy of the Research
Fast forward to today, and the implications of this case still resonate. It serves as a cautionary tale about the lengths to which medical research can go and the responsibilities of researchers to uphold ethical standards. As we navigate advancements in medicine, we must continually engage in conversations about what it means to respect human life and dignity.
The research conducted in this case may have contributed to advancements in the understanding of pediatric brain death and neurological functions, but at what cost? The ethical implications extend beyond just this one incident, prompting medical professionals, ethicists, and society at large to reflect on how we treat the deceased and the moral responsibilities we have toward them.
Public Reaction and Awareness
The story of the young boy from Nebraska has sparked significant public interest and discussion. As more people learn about this case, it raises awareness about the ethical dilemmas surrounding medical research. Public discourse is essential for holding the medical community accountable and ensuring that ethical standards are upheld.
Many advocates for ethical medical practices emphasize the importance of transparency in research. Families should be aware of what happens to their loved ones after death, particularly in cases where bodies are used for research purposes. This case has led to calls for clearer laws and regulations surrounding post-mortem research and consent.
The story encourages a broader conversation about the intersection of science and ethics. When it comes to medical advancements, the end does not always justify the means. Society must grapple with the complexities of medical research and ensure that ethical principles are at the forefront of discussions.
Conclusion
The tragic story of a four-year-old boy from Nebraska, declared brain dead in 1983 and kept “alive” for over 20 years for research, compels us to reflect on the intersection of medical research, ethics, and human dignity. As we continue to advance in the field of medicine, we must prioritize ethical considerations, ensuring that respect for the deceased and their families remains paramount. This case serves as a poignant reminder of the delicate balance between the pursuit of knowledge and the sanctity of human life, urging us to tread carefully as we navigate the complexities of medical research.