Texas Bill SB2422: Scrubbing Controversial Drug Records?
Texas Bill SB2422: A Legislative Overview
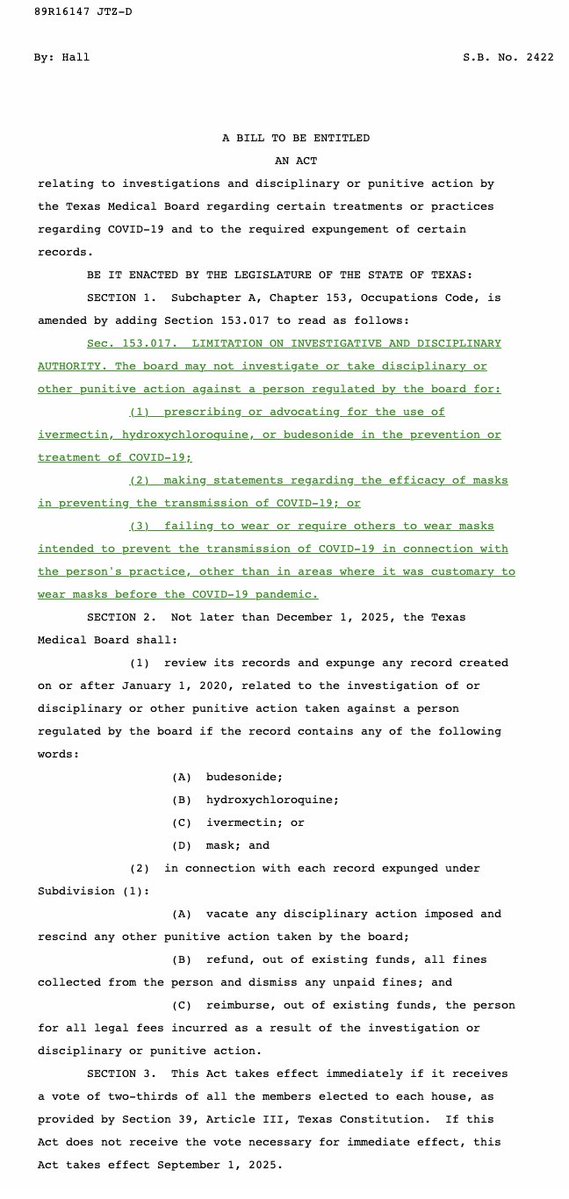
In March 2025, the Texas Medical Board was thrust into the spotlight with the introduction of Senate Bill SB2422. This proposed legislation aims to bring significant changes to how the Texas Medical Board manages records related to investigations, disciplinary actions, and other punitive measures against medical professionals. The focal point of this bill is the expungement of records that include specific terms associated with certain medications and treatments.
Key Provisions of SB2422
SB2422 is designed to expunge any record related to an investigation or disciplinary action taken against a medical professional if that record contains specific keywords. The bill highlights three particular substances:
- Budesonide
- Hydroxychloroquine
- Ivermectin
These medications have garnered considerable attention in the context of various health discussions, particularly during the COVID-19 pandemic. By mandating the expungement of records mentioning these drugs, the bill aims to protect medical professionals from potential repercussions tied to their use of these treatments.
Implications for Medical Professionals
The implications of SB2422 are far-reaching for healthcare providers in Texas. By expunging records that include these terms, the bill is intended to shield practitioners from negative evaluations or disciplinary actions associated with their prescribing practices or treatment recommendations.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
This could lead to a more favorable environment for physicians who have utilized these medications in their practice, particularly in the context of controversial treatments that have been both supported and criticized in medical communities.
Protecting Medical Autonomy
One of the primary arguments in favor of SB2422 is the protection of medical autonomy. Advocates assert that physicians should have the freedom to make clinical decisions based on their assessments rather than fear repercussions for using certain medications, especially those that have sparked public debate.
Supporters believe that the bill could encourage doctors to explore alternative treatment options without the fear of facing disciplinary actions. This could ultimately lead to more personalized and potentially innovative approaches to patient care.
Controversy Surrounding the Bill
Despite its intentions, SB2422 has not been without controversy. Critics argue that expunging records related to the use of these medications could undermine accountability within the medical profession. They voice concerns that the bill may enable the continued prescription of treatments that lack robust clinical support, potentially endangering patients’ health.
Furthermore, the bill raises questions about the transparency of the medical profession. By removing records of investigations and disciplinary actions, there is a concern that patients may not have access to crucial information about their healthcare providers’ histories, which could impact their trust in the healthcare system.
The Role of the Texas Medical Board
The Texas Medical Board plays a crucial role in overseeing the licensing and regulation of medical professionals in the state. The introduction of SB2422 will require the Board to adapt its policies and procedures regarding record-keeping and disciplinary actions.
If enacted, the Board will have to establish clear guidelines for implementing the expungement process outlined in the bill. This may involve creating a framework for determining which records qualify for expungement and ensuring that the process is conducted fairly and transparently.
Broader Context: The Use of Controversial Medications
The medications mentioned in SB2422—budesonide, hydroxychloroquine, and ivermectin—have been at the center of significant public and medical debate, especially during the COVID-19 pandemic.
- Budesonide is a corticosteroid used to treat various conditions, including asthma and inflammatory bowel disease. Its use in COVID-19 has been explored, but the evidence remains mixed.
- Hydroxychloroquine gained notoriety as a potential COVID-19 treatment, leading to widespread use despite mixed clinical trial results. Its usage has been heavily scrutinized, and the FDA ultimately revoked its emergency use authorization for COVID-19 treatment.
- Ivermectin, an antiparasitic medication, has also been promoted for COVID-19 treatment without sufficient scientific backing, leading to widespread controversy and debate.
By focusing on these medications, SB2422 reflects the ongoing tensions within the medical community regarding treatment options and the role of governmental oversight.
Conclusion: The Future of SB2422
As SB2422 moves through the legislative process, it will undoubtedly continue to spark discussions about medical accountability, treatment autonomy, and the proper balance between regulation and professional freedom.
The potential expungement of records related to the use of budesonide, hydroxychloroquine, and ivermectin raises important questions about the future of medical practice in Texas. Advocates for the bill argue that it will foster an environment of innovation and patient-centered care, while critics caution against potential risks to patient safety and transparency.
Ultimately, the outcome of SB2422 could set a significant precedent for how medical records are handled in Texas, influencing both practitioners and patients for years to come. As the legislative process unfolds, stakeholders across the healthcare spectrum will be closely monitoring the developments surrounding this pivotal bill.
For further updates on the progression of Texas Senate Bill SB2422, it is advisable to follow reputable news sources and official legislative channels to stay informed about its implications for the healthcare community in Texas.

TX bill SB2422 would require Texas Medical Board to expunge any record related to the investigation of or disciplinary or other punitive action taken against a person if the record contains any of the following words: (A) budesonide (B) hydroxychloroquine; (C) ivermectin; or… pic.twitter.com/nFOsaSyqhb
— Mary Talley Bowden MD (@MdBreathe) March 24, 2025
Understanding TX Bill SB2422: A Closer Look
It’s no secret that the landscape of healthcare regulation is continually evolving, especially in response to recent global health crises. One such legislative measure that has sparked a significant amount of discussion is the TX bill SB2422. This proposed legislation aims to influence how the Texas Medical Board handles certain medical records. Specifically, it would mandate the expungement of any records related to investigations or disciplinary actions against physicians if those records mention specific medications. Let’s dive deeper into what this means.
What Does TX Bill SB2422 Propose?
TX bill SB2422 would require the Texas Medical Board to expunge any record related to the investigation of or disciplinary or other punitive action taken against a person if the record contains any of the following words: (A) budesonide, (B) hydroxychloroquine, and (C) ivermectin. This proposal raises numerous questions about its implications for public health, medical practice, and patient safety.
The Medications in Focus: Budesonide, Hydroxychloroquine, and Ivermectin
Before we delve into the implications of this bill, it’s essential to understand the medications that are at the center of this discussion.
– **Budesonide** is a corticosteroid used to treat various conditions, including asthma and inflammatory bowel disease. In recent years, it has garnered attention for its potential use in managing COVID-19 symptoms.
– **Hydroxychloroquine**, traditionally used to treat malaria and autoimmune diseases, became a controversial topic during the COVID-19 pandemic when some touted it as a potential treatment for the virus, despite limited evidence.
– **Ivermectin**, another drug with a long history of use against parasitic infections, also entered the spotlight during the pandemic as a suggested treatment for COVID-19, leading to a surge in prescriptions even when its efficacy for this purpose was widely debated.
Each of these medications has been subject to intense scrutiny and discussion, particularly in the context of COVID-19 treatment.
The Rationale Behind the Bill
Proponents of TX bill SB2422 argue that it seeks to protect physicians from punitive actions that may arise from their attempts to prescribe these medications in good faith. They believe that the bill promotes clinical autonomy and allows doctors to make decisions without fear of retribution from regulatory bodies. The idea is that if doctors are discouraged from prescribing these medications due to fear of disciplinary action, patients may be deprived of potential treatment options.
However, critics raise concerns about the potential risks of this legislation. They argue that expunging records related to the investigation of these medications could lead to a lack of accountability for physicians. If certain treatments are not supported by robust evidence, allowing doctors to prescribe them without oversight may pose risks to patient safety.
Legal and Ethical Considerations
The implications of TX bill SB2422 extend beyond immediate medical practice; they raise significant legal and ethical questions. For one, how does this bill align with the principles of informed consent and patient safety? Patients have the right to be informed about the medications they are prescribed, including the potential risks and benefits. If a physician’s record is expunged for prescribing a medication that is later deemed ineffective or harmful, what does that mean for the accountability of the medical professional?
Moreover, the ethical implications of such legislation are profound. Medical professionals are bound by their Hippocratic Oath to do no harm. If the Texas Medical Board cannot take action against practitioners who may be providing treatments without sufficient evidence, it could undermine the trust that patients place in the medical system.
The Public Reaction and Ongoing Debate
As is often the case with contentious legislative proposals, public reaction to TX bill SB2422 has been mixed. Supporters argue that it champions medical freedom and protects doctors who are navigating uncharted waters in an unprecedented health crisis. They contend that the medical community should be allowed to explore all potential treatment options for patients, especially when facing a novel virus like COVID-19.
On the flip side, opponents voice concerns about the potential for misuse of the bill. They worry that it could lead to an environment where unproven or even dangerous treatments are prescribed without appropriate oversight. As discussions continue, it’s clear that the debate surrounding TX bill SB2422 is emblematic of broader tensions in healthcare today—namely, the balance between regulatory oversight and the autonomy of medical professionals.
What’s Next for TX Bill SB2422?
As TX bill SB2422 makes its way through the legislative process, it’s essential to keep a close eye on how it evolves. Lawmakers will undoubtedly face pressure from both sides of the argument, and the final outcome will likely reflect a compromise between the desire for medical freedom and the need for patient safety.
Stakeholders, including healthcare professionals, patients, and advocacy groups, must remain engaged in this discussion. Open dialogue and collaboration can help ensure that any legislative measures prioritize both the autonomy of physicians and the safety of patients.
Conclusion: The Future of Medical Regulation in Texas
The introduction of TX bill SB2422 highlights the complexities of medical regulation in today’s world. As we navigate the uncertain waters of healthcare, it’s crucial to strike a balance that respects the expertise of medical professionals while protecting patient safety. The ongoing discussions surrounding this bill underscore the importance of transparency, accountability, and informed decision-making in the medical field.
As Texas moves forward with this bill, one thing is clear: the conversation about the regulation of medical practices and the autonomy of healthcare providers is far from over. Whether this legislation will ultimately benefit or hinder the practice of medicine remains to be seen, but it undeniably represents a pivotal moment in the ongoing dialogue about healthcare in America.