“Shocking Study Reveals 30x death Risk for Young Males After 5 Vaccines!”
epidemiology risk analysis, vaccine side effects research, young adult mortality statistics
—————–
Understanding Epidemiological Risk: The Implications of High Hazard Ratios in Vaccine Studies
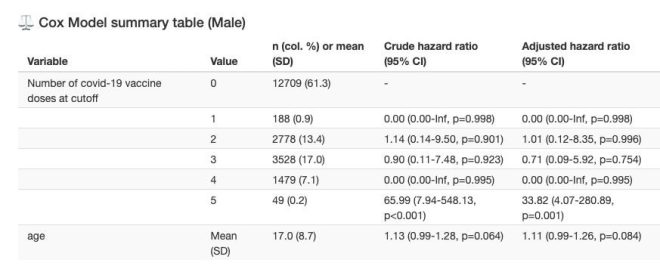
In recent discussions surrounding vaccine safety, a tweet by Steve Kirsch has sparked significant interest and concern, particularly regarding the long-term effects of COVID-19 vaccinations among young males. Kirsch’s tweet highlights a staggering hazard ratio (HR) greater than 30, suggesting a 30-fold increase in the risk of death among males aged 0 to 30 who have received five doses of the vaccine. This summary aims to delve into the implications of such findings, the context behind hazard ratios in epidemiology, and the broader conversation surrounding vaccine safety.
What is Hazard Ratio (HR)?
A hazard ratio is a measure used in epidemiology to compare the hazard (or risk) of an event occurring in two different groups. It is commonly used in clinical trials and observational studies to assess the effect of a treatment or intervention. An HR greater than 1 indicates an increased risk in the treatment group compared to the control group. Conversely, an HR less than 1 suggests a reduced risk.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
In the context of Kirsch’s statement, an HR greater than 30 is exceptionally rare and raises alarm bells in the epidemiological community. Such a high ratio indicates that the risk of death for this specific demographic is dramatically elevated compared to those who have not received the vaccine.
The Significance of the Data
Kirsch references data from Japan, emphasizing its statistical significance. Statistical significance is crucial in epidemiology as it helps determine whether the observed effects are likely due to chance or represent a true association. With highly significant results, the findings suggest a robust correlation between the number of vaccine doses and increased mortality risk in the specified age group.
This revelation has ignited debates regarding vaccine policies, especially as it pertains to young adults who are generally considered to be at lower risk for severe outcomes from COVID-19. The implications of such data could lead to calls for re-evaluation of vaccination strategies, particularly concerning booster doses and their necessity in younger populations.
Analyzing the Context
To fully comprehend the implications of Kirsch’s tweet, it is essential to consider the broader context of vaccine development and safety monitoring. Vaccines undergo rigorous testing and evaluation before approval, and ongoing surveillance continues post-approval to monitor adverse effects. However, as with any medical intervention, rare side effects may not be immediately apparent during clinical trials which typically involve a limited number of participants.
The discussion surrounding vaccine safety is particularly relevant in the age of social media, where information (and misinformation) can spread rapidly. It is crucial for the scientific community to communicate transparently about the risks and benefits of vaccination, especially as new data emerges.
The Broader Vaccine Safety Conversation
The emergence of significant findings such as those presented by Kirsch raises important questions about vaccine safety protocols and the need for continuous research. Public health agencies and scientists must remain vigilant in assessing the long-term effects of vaccines, particularly for specific demographics that may respond differently to vaccinations.
While the focus has primarily been on combating the COVID-19 pandemic, the implications of such studies should not only be about immediate public health responses but also about the future of vaccine development. Continuous monitoring and research are essential to ensure that vaccines remain safe for all populations, particularly vulnerable groups.
The Importance of Reliable Sources
In light of social media’s influence on public perception of health information, it’s vital for individuals to seek out reliable and scientifically validated sources when interpreting data such as that shared by Kirsch. Peer-reviewed studies, expert opinions, and public health guidelines should form the backbone of any discussions surrounding vaccine safety.
Misinformation can lead to vaccine hesitancy, which poses a significant risk to public health efforts aimed at controlling infectious diseases. Therefore, understanding the data, its context, and the scientific consensus is essential for making informed decisions about vaccinations.
Conclusion
The alarming hazard ratio of over 30 presented by Steve Kirsch raises critical discussions about the safety of vaccines, particularly concerning young males who have received multiple doses. While the data indicates a significant risk of mortality, it is essential to analyze such findings within the broader context of vaccine development, safety monitoring, and public health responses.
As the conversation continues, it is crucial for the scientific community to address these concerns transparently and ensure that the public has access to accurate, evidence-based information. Ongoing research and monitoring are necessary to understand the long-term implications of vaccinations and to maintain public trust in vaccination programs.
In conclusion, while data like that shared by Kirsch can be alarming, it serves as a reminder of the need for rigorous scientific evaluation and communication in the ever-evolving landscape of public health. Only through informed discussions and research can we navigate the complexities of vaccine safety and efficacy, ultimately protecting public health while ensuring the safety of our populations.

BREAKING: HR > 30 is rarely seen in epidemiology.
That’s a 30x increase in the risk of death.
The Japanese data shows this level of harm for 0 to 30 year-old males who got five shots. Highly statistically significant. pic.twitter.com/7F6lZnOJTa
— Steve Kirsch (@stkirsch) June 27, 2025
BRAKING: HR > 30 is Rarely Seen in Epidemiology
When it comes to epidemiology, seeing a hazard ratio (HR) greater than 30 is quite rare. This isn’t just a number; it represents a significant shift in our understanding of risk factors, particularly in relation to health outcomes. The implications of such a statistic can be staggering, especially when it concerns the risk of death. Imagine a scenario where a specific group experiences a 30-fold increase in the likelihood of dying. It’s a wake-up call for researchers, healthcare professionals, and the public alike.
Understanding Hazard Ratios
So, what exactly is a hazard ratio? In simple terms, it compares the risk of an event occurring in two different groups. A HR of 1 means there’s no difference in risk, while a HR greater than 1 indicates increased risk. When we talk about a HR exceeding 30, we are venturing into an alarming territory that demands immediate attention and further investigation.
The Shocking Increase in Risk
According to recent data shared by Steve Kirsch, we’re looking at a 30x increase in the risk of death for a very specific group: young males aged 0 to 30 who received five shots of a certain vaccine. This finding is not only startling but also highly statistically significant. The implications of this data could affect health policies and public perception regarding vaccinations.
The Japanese Data and Its Findings
The research in question comes from Japan, where data has shown concerning trends among young males who received multiple vaccine doses. This data is crucial because it highlights a potential correlation between vaccine administration and heightened health risks. The numbers tell a compelling story that cannot be ignored. Understanding the context of this data is vital for both public health officials and the general public.
What Does This Mean for Young Males?
For young males, particularly those aged 0 to 30, these findings raise critical questions. How can a vaccine, which is generally seen as a protective measure, lead to such alarming statistics? It’s essential to engage with this data thoughtfully and consider the broader implications. Parents and guardians are likely to feel concerned, and rightly so. The balance between protecting against diseases through vaccination and understanding potential risks is a conversation that needs to happen.
Exploring Potential Causes
While the statistics are clear, the underlying causes are still being explored. Scientists and researchers are scrutinizing various factors that could contribute to this increase in risk. Is it related to the specific type of vaccine? What about genetic predispositions or underlying health conditions? These questions are crucial as they shape future research and health recommendations.
The Importance of Continuous Research
As alarming as these findings are, it’s essential to recognize that continuous research is vital. The scientific community must dive deeper into these statistics to understand their implications fully. This isn’t about creating panic but rather about fostering an informed public discourse. Vaccinations have been a cornerstone of public health, and understanding the nuances of their effects is critical.
Public Response to the Data
Public reaction to such findings can be mixed. Some people may question the efficacy and safety of vaccines, while others may feel that the benefits outweigh the risks. It’s a delicate balance between public health messaging and individual fear, and navigating this landscape requires sensitivity and transparency from health officials.
The Role of Social Media in Health Information
In an age where information travels at lightning speed, social media plays a massive role in how health data is disseminated and perceived. The tweet from Steve Kirsch exemplifies how quickly information can spread and the kind of reactions it can elicit. Social media can be a double-edged sword; it can raise awareness but can also lead to misinformation if not handled correctly.
Future Directions for Research and Policy
As we move forward, it’s crucial that researchers prioritize understanding this data. Health policies may need to be revisited in light of these findings, especially concerning vaccination protocols for young males. Collaboration between scientists, healthcare providers, and policymakers will be essential in addressing these concerns and implementing effective strategies.
Engaging with the Community
For individuals and families, engaging with trusted healthcare professionals is vital. If you have concerns about vaccinations or health risks, don’t hesitate to seek out information from credible sources. The dialogue surrounding health and vaccines should be open and honest, allowing for questions and discussions that lead to informed decisions.
Conclusion: Navigating Uncertainty in Health
The data emerging from Japan is a stark reminder of the complexities we face in public health. While vaccines have undoubtedly saved countless lives, understanding the potential risks associated with them is equally important. As we navigate this uncertain territory, let’s ensure that our conversations are rooted in facts and a shared commitment to health and safety.
In a world where health data can change rapidly, staying informed is your best defense. Whether you’re a parent, a young adult, or simply someone concerned about public health, keeping an eye on emerging research and engaging in community discussions will empower you to make the best choices for your health.
“`
This article is designed to engage readers, using a conversational tone while providing them with essential information about the significant findings related to hazard ratios in epidemiology. It emphasizes the importance of understanding the data and encourages informed discussions around health and vaccinations.
