“Massachusetts’ Covid Response: A deadly Legacy Ranked Third Worst Globally!”
Covid death rates, Massachusetts pandemic response, public health impact
—————–
Massachusetts COVID-19 Response: Analyzing the Third Worst Death Rate in the World
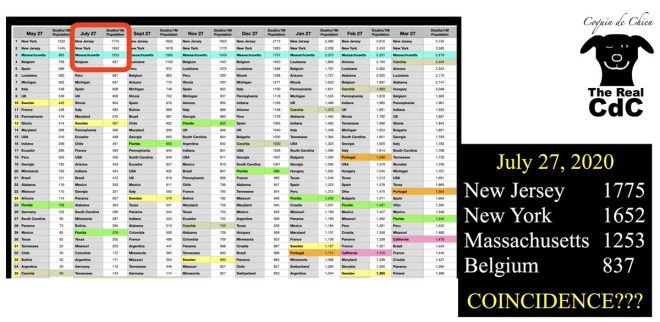
The COVID-19 pandemic has highlighted various responses by governments worldwide, and Massachusetts has been a focal point for debate regarding its handling of the crisis. According to a tweet by John Beaudoin, Massachusetts reportedly ranks as having the third worst COVID-19 death rate per capita globally after the first year of the pandemic. This alarming statistic has raised serious questions about the efficacy of the state’s response and strategies implemented to mitigate the virus’s spread.
Understanding the Rankings
The claim that Massachusetts holds the third-worst position for COVID-19 deaths per population is significant and warrants thorough examination. This statistic places Massachusetts alongside New York and New Jersey, which are also cited as having extremely high death rates due to the pandemic. The ranking is not merely a statistic; it reflects public health decisions, resource allocation, and the overall effectiveness of the state’s response.
The Context of COVID-19 in Massachusetts
When the COVID-19 outbreak began in early 2020, Massachusetts was quick to implement measures aimed at curbing the spread of the virus. These included stay-at-home orders, business closures, and mask mandates. However, as the pandemic progressed, evidence emerged suggesting that the state’s response may have inadvertently contributed to the high mortality rate. Critics argue that certain policies, especially those concerning nursing homes and vulnerable populations, were inadequately planned and executed.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
Key Factors Contributing to High Death Rates
- Nursing Home Policies: One of the most contentious aspects of Massachusetts’ COVID-19 response has been its policies regarding nursing homes. Early in the pandemic, the state mandated that nursing homes accept COVID-19 positive patients, which some experts believe led to widespread outbreaks in these facilities. With a significant portion of COVID-19 deaths occurring among elderly individuals in nursing homes, this policy has been heavily scrutinized.
- Testing and Resources: The availability of testing and healthcare resources played a critical role in managing the pandemic. Massachusetts faced challenges in scaling up testing capacity quickly, which limited the ability to identify and isolate cases early on. This delay likely contributed to the virus spreading unchecked, leading to higher mortality rates.
- Public Messaging and Compliance: Effective communication and public compliance are vital during a health crisis. In Massachusetts, mixed messages regarding safety guidelines and reopening phases may have led to confusion among the population. This uncertainty can result in reduced adherence to health protocols, thereby exacerbating the spread of the virus.
Comparing Massachusetts to Other States
When comparing Massachusetts’ COVID-19 response to that of other states, particularly New York and New Jersey, several patterns emerge. Both neighboring states faced similar challenges but also implemented differing strategies. For instance, while New York and New Jersey experienced high death rates, they also introduced aggressive measures to increase hospital capacity and testing, which may have mitigated further loss of life.
Reactions and Accountability
The high death rates in Massachusetts have led to significant public outcry and demands for accountability from state leaders. Many citizens and health experts argue that the state must learn from these mistakes to prevent similar outcomes in future public health crises. Investigations and reviews of the decisions made during the pandemic are ongoing, with the goal of improving response protocols and safeguarding vulnerable populations in the future.
The Path Forward
As Massachusetts moves forward, addressing the lessons learned from the COVID-19 pandemic will be crucial. This includes:
- Enhancing Public Health Infrastructure: Strengthening the public health system is vital to ensure preparedness for any future pandemics. This could involve investing in healthcare resources, improving data analytics for tracking disease spread, and ensuring adequate support for nursing homes and long-term care facilities.
- Improving Communication: Clear and consistent messaging from health officials and government leaders can help build public trust and compliance with health guidelines. Educational campaigns about the importance of vaccinations, masking, and social distancing are essential as the state continues to recover.
- Focusing on Vulnerable Populations: Special attention must be given to vulnerable populations, particularly the elderly and those with pre-existing health conditions. Policies should prioritize their safety and well-being, ensuring that they receive the necessary support and care during a health crisis.
Conclusion
The COVID-19 pandemic has exposed vulnerabilities within public health systems across the globe, and Massachusetts is no exception. Ranking as having the third worst COVID-19 death rate per population is a stark reminder of the complexities and challenges faced in managing a public health emergency. As discussions continue regarding the effectiveness of the state’s response, it is imperative for stakeholders to take a comprehensive approach to enhance future preparedness. By learning from past mistakes, Massachusetts can work towards ensuring a healthier future for all its residents.
In summary, the examination of Massachusetts’ COVID-19 response is a crucial part of understanding the broader implications of public health management. The state must leverage this experience to build a more resilient healthcare system, ensuring better outcomes in future crises.

1/
Massachusetts purports the THIRD worst Covid deaths per population in the ENTIRE WORLD after the first year of Covid.Third WORST BY FAR sovereign in the world. Massachusetts’ response killed MORE PEOPLE by their Covid response than any other sovereign except NY and NJ pic.twitter.com/afU5HPcVyb
— John Beaudoin, Sr., The Real CdC, The Last Boomer (@JohnBeaudoinSr) June 21, 2025
Massachusetts Purports the THIRD Worst Covid Deaths per Population in the Entire World After the First Year of Covid
The Covid-19 pandemic was nothing short of a global crisis, impacting lives and economies across the world. As we reflect on the past years, one thing stands out: the staggering death tolls that some regions experienced due to their pandemic response. Massachusetts, a state known for its rich history and academia, now finds itself in the spotlight for a rather disheartening reason. According to a tweet by John Beaudoin, Massachusetts ranks as the *third worst* in the world for Covid deaths per population after the first year of the pandemic.
This statistic isn’t just a number; it’s a wake-up call. When we look closely, we see that the state’s response to the pandemic has been criticized for leading to higher mortality rates than many others, including New York and New Jersey. But how did Massachusetts end up in this grim position?
Third WORST By Far Sovereign in the World
When we talk about sovereign states, we usually think about countries, but here, we’re referring to states like Massachusetts that have their own governance structures. The claim of being the *third worst* is not just an isolated incident; it reflects broader systemic issues within public health management during a crisis.
Massachusetts’ strategy involved a mix of stringent lockdowns and public health mandates aimed at curbing the virus’s spread. However, as the data shows, these efforts may not have been as effective as intended. The state’s high population density, especially in urban areas like Boston, compounded the crisis, making it easier for the virus to spread. Notably, vulnerable populations, particularly in nursing homes, faced the brunt of the devastation.
The Department of Public Health in Massachusetts has been under scrutiny for how it handled the crisis. Reports indicated that a significant proportion of deaths occurred in long-term care facilities. According to a [report by the Boston Globe](https://www.bostonglobe.com), a large percentage of the Covid-19 deaths in the state were linked to nursing homes, which raises questions about the adequacy of the response to protect these vulnerable populations.
Massachusetts’ Response Killed More People by Their Covid Response Than Any Other Sovereign Except NY and NJ
Critics often point to the decisions made during the pandemic as pivotal moments that impacted the death toll. Massachusetts, along with New York and New Jersey, faced immense criticism for its handling of the pandemic. The decisions made in the early days of Covid-19, particularly around hospital admissions and nursing home policies, are often cited as having fatal consequences.
For instance, early in the pandemic, some policies allowed Covid-positive patients to be discharged to nursing homes, which led to catastrophic outbreaks in these facilities. This decision has been a focal point in discussions about how Massachusetts’ response contributed to its high death rate. The [New York Times](https://www.nytimes.com) reported that nursing homes across the state struggled with inadequate staffing and resources, further exacerbating the crisis.
It’s essential to highlight that while the intent behind these policies was to alleviate hospital overcrowding, the execution left much to be desired. The long-term implications of these decisions continue to be felt today, as families mourn the loss of loved ones and communities grapple with the aftermath.
Public Perception and Policy Changes
As more data became available, public sentiment shifted. Many Massachusetts residents expressed frustration over the perceived failures of their leaders. Trust in public health officials waned as families sought answers regarding the tragic loss of life.
In response to the mounting criticism, Massachusetts lawmakers have since proposed various reforms aimed at improving the state’s public health infrastructure. These reforms include reviewing nursing home policies, increasing funding for health services, and enhancing support for vulnerable communities.
A [report from WBUR](https://www.wbur.org) highlights that state officials are now focusing on improving transparency and accountability in the health system. The hope is that by learning from past mistakes, Massachusetts can better prepare for any future health crises.
The Importance of Learning from the Past
When looking at the Covid pandemic, it’s crucial to remember that hindsight is 20/20. However, as Massachusetts grapples with the implications of its response, it serves as a reminder that every decision has consequences. While some states managed to keep their death tolls lower through various strategies, others, like Massachusetts, found themselves facing harsh realities.
The lessons learned from this crisis are invaluable. Moving forward, Massachusetts can take proactive steps to ensure that public health policies prioritize the well-being of all residents, particularly the most vulnerable. The emphasis should be on creating a robust response framework that can adapt to rapidly changing situations, ensuring that no community is left behind.
Community Resilience and Recovery
Despite the challenges faced during the pandemic, Massachusetts has shown incredible resilience. Communities came together to support each other, whether through mutual aid networks, volunteer programs, or simply by checking in on neighbors. This spirit of unity is what will ultimately help the state heal and rebuild.
As we continue to navigate the post-pandemic world, it’s essential to recognize the importance of community engagement in public health. Local organizations, non-profits, and community leaders have played a crucial role in disseminating information, providing resources, and advocating for those most affected by the crisis.
By fostering strong community ties and empowering local voices, Massachusetts can create a more inclusive and effective public health strategy moving forward.
Conclusion: Moving Forward Together
Massachusetts’ experience during the Covid-19 pandemic highlights the complexities of managing public health crises. While the state currently holds the unfortunate title of having the *third worst Covid deaths per population* in the world, it also represents an opportunity for growth and improvement.
By learning from past mistakes, increasing transparency, and focusing on community-driven solutions, Massachusetts can emerge stronger and more resilient. The journey ahead may be challenging, but with collective effort and commitment to public health, the state can ensure a brighter future for all its residents.
In the end, it’s not just about the numbers; it’s about the lives behind those numbers and the lessons we carry forward. The tragedy of Covid-19 must serve as a catalyst for meaningful change, ensuring that we are better prepared for whatever challenges lie ahead.
