Death- Obituary News
Understanding the Transition from Severe Sepsis to Septic Shock
In recent years, the medical community has witnessed significant changes in the way we understand and classify sepsis, particularly severe sepsis. A tweet from Ngouagna Frank, which sparked conversation, proclaimed, "Severe sepsis is dead," highlighting a pivotal shift in sepsis terminology and treatment protocols. This summary explores the implications of this statement, the evolution of sepsis definitions, and the critical importance of recognizing septic shock.
What is Sepsis?
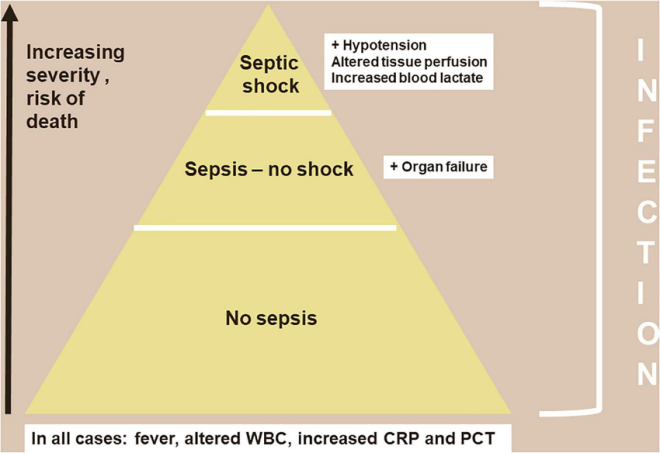
Sepsis is a life-threatening condition that arises when the body’s response to an infection injures its tissues and organs. It can lead to septic shock, characterized by a significant drop in blood pressure and the potential for multiple organ failure. Traditionally, sepsis was categorized into stages, including sepsis, severe sepsis, and septic shock. However, the definitions have evolved over time to simplify understanding and improve clinical outcomes.
The Evolution of Sepsis Classification
Historically, severe sepsis was defined as sepsis accompanied by organ dysfunction, hypoperfusion, or hypotension. However, in 2016, the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) redefined these classifications. The new definition eliminated the term "severe sepsis" altogether, focusing instead on the continuum of sepsis leading directly to septic shock.
- YOU MAY ALSO LIKE TO WATCH THIS TRENDING STORY ON YOUTUBE. Waverly Hills Hospital's Horror Story: The Most Haunted Room 502
This change was made to streamline the understanding of sepsis and to ensure that healthcare providers could more effectively identify and treat patients. By eliminating "severe sepsis" from the terminology, the medical community aims to reduce confusion and enhance the urgency with which sepsis is treated.
The Importance of Recognizing Septic Shock
As sepsis progresses, it can lead to septic shock, a critical state where the body’s blood pressure drops dangerously low. This condition requires immediate medical intervention, often including intravenous fluids and medications to stabilize the patient. Recognizing the signs of septic shock is crucial for timely treatment and improving patient outcomes.
Common symptoms include:
- Confusion or disorientation
- Rapid heart rate
- Shortness of breath
- Extreme weakness or fatigue
- Skin that appears pale or mottled
Understanding the progression from sepsis to septic shock is vital for healthcare professionals and caregivers alike. The focus should be on early detection, rapid assessment, and immediate intervention to manage the condition effectively.
The Impact of the New Definition on Treatment Protocols
The elimination of severe sepsis from clinical guidelines has profound implications for treatment protocols. With the focus shifting towards identifying sepsis and its progression to septic shock, healthcare providers are encouraged to act quickly, ensuring that patients receive the necessary interventions without delay.
This shift also emphasizes the importance of using the Sequential Organ Failure Assessment (SOFA) score to assess the degree of organ dysfunction. The SOFA score helps clinicians evaluate the severity of sepsis and guide treatment decisions based on the patient’s specific needs.
Public Awareness and Education
While medical professionals are adapting to the new definitions and protocols, public awareness is equally important. Understanding the signs and symptoms of sepsis can lead to faster recognition and treatment. Educational campaigns aimed at both healthcare providers and the general public can help improve outcomes by ensuring that individuals know when to seek medical attention.
The Future of Sepsis Management
As research continues, the medical community is committed to refining the definitions and treatment approaches for sepsis. Ongoing studies aim to identify biomarkers that can predict the progression of sepsis, allowing for even more targeted and effective interventions.
Moreover, there is a push for more comprehensive training for healthcare providers, ensuring they are equipped to recognize and treat sepsis at all stages. This includes not only the clinical aspects but also the emotional support for patients and families affected by this serious condition.
Conclusion: A Call to Action
The statement "Severe sepsis is dead" encapsulates a significant shift in our understanding of sepsis and its implications for treatment. By focusing on sepsis and septic shock as interconnected stages, the medical community aims to enhance patient care and improve outcomes.
As we move forward, it is crucial for both healthcare providers and the public to stay informed about the signs, symptoms, and treatment options for sepsis. Early recognition, timely intervention, and continued education are vital components in the fight against this life-threatening condition.
In conclusion, while the terminology and definitions may change, the urgency of addressing sepsis remains. With a commitment to ongoing education and improved clinical practices, we can work towards reducing the impact of sepsis and saving lives.

Severe sepsis is dead
RIPhttps://t.co/ILykYhFQBX pic.twitter.com/SS6SFS4N7l— Ngouagna Frank (@zngouagna) February 23, 2025
Severe Sepsis is Dead
In recent discussions surrounding critical health issues, a poignant tweet from Ngouagna Frank stirred quite a conversation: “Severe sepsis is dead. RIP.” This bold statement wasn’t just a casual remark; it sparked an essential dialogue about the evolving understanding of severe sepsis and its treatment. So, what does this mean in the context of medical advancements and patient care?
Understanding Severe Sepsis
Before diving into the implications of Frank’s statement, it’s crucial to understand what severe sepsis is. Sepsis, often referred to as a “silent killer,” occurs when the body’s response to infection spirals out of control, leading to systemic inflammation. This can result in organ failure and, ultimately, death if not treated promptly. Severe sepsis is a heightened level of this condition, where the body’s organs begin to fail, necessitating immediate medical intervention.
The Shift in Medical Perspective
The assertion that “severe sepsis is dead” can be interpreted as a reflection of the ongoing transformation in how the medical community perceives and treats sepsis. Over the years, research has illuminated new approaches, therapies, and guidelines that have significantly improved patient outcomes. For instance, early recognition and prompt treatment with antibiotics and fluids are now cornerstones of managing sepsis effectively.
RIP: A Call for Change
The phrase “RIP” in the tweet isn’t just a farewell to severe sepsis as a condition; it’s a rallying cry for medical professionals to rethink their strategies. The traditional methods of treating sepsis have faced scrutiny as new evidence emerges. Studies have shown that the early administration of broad-spectrum antibiotics and aggressive fluid resuscitation can drastically alter the course of the disease. This shift aims to reduce mortality rates associated with severe sepsis.
Advancements in Treatment Protocols
One of the most significant changes in treating severe sepsis comes from the implementation of sepsis bundles, which are sets of guidelines designed to streamline and improve care. These bundles emphasize the importance of timely interventions, such as administering antibiotics within the first hour of recognizing sepsis symptoms. This proactive approach has proven to be a game-changer, resulting in better outcomes for patients.
Raising Awareness and Education
Awareness plays a vital role in combating sepsis. Many people are unaware of the early signs, which can include fever, increased heart rate, confusion, and shortness of breath. Education initiatives aimed at both healthcare providers and the general public are essential in ensuring that sepsis is recognized and treated early. Organizations like the Sepsis Alliance work tirelessly to promote awareness and provide resources for both patients and medical professionals.
The Role of Technology in Fighting Sepsis
With the rise of technology in healthcare, tools like electronic health records (EHR) and sepsis prediction algorithms are becoming integral in identifying at-risk patients. These systems can analyze patient data in real-time to flag potential cases of sepsis, allowing for quicker responses from medical teams. This proactive approach aligns with the tweet’s sentiment, as it represents a shift away from traditional methods towards innovative solutions.
Future Directions and Research
As we consider the statement “severe sepsis is dead,” it’s important to acknowledge that the fight against sepsis is ongoing. Research continues to explore new therapies, including immunotherapy and the use of biomarkers to identify sepsis more accurately. The medical community is committed to developing more effective treatments and improving survival rates, ensuring that the phrase “severe sepsis is dead” reflects a genuine advancement in understanding and managing this critical condition.
Global Impact of Severe Sepsis
Sepsis does not discriminate; it affects millions of individuals worldwide, making it a significant public health concern. The World Health Organization (WHO) recognizes sepsis as a global health priority and emphasizes the need for comprehensive strategies to address it. These strategies include improving access to healthcare, enhancing infection prevention measures, and ensuring that healthcare providers are trained to recognize and treat sepsis effectively.
Patient Stories and Experiences
Personal stories about sepsis often highlight the urgency of recognition and treatment. Patients and their families frequently share their harrowing experiences, which serve as powerful reminders of the condition’s severity. These narratives can help to humanize the statistics and drive home the importance of awareness and education. They also underscore the necessity for healthcare systems to prioritize rapid response protocols to save lives.
Conclusion: A New Dawn for Sepsis Management
The tweet from Ngouagna Frank encapsulates a significant moment in the evolution of sepsis treatment. While the phrase “severe sepsis is dead” may appear stark, it symbolizes hope and progress in the fight against this life-threatening condition. As we continue to learn and adapt in the medical field, the ultimate goal remains the same: to reduce mortality rates and improve the quality of life for those affected by sepsis.
In this ever-evolving landscape, staying informed and engaged is crucial. Whether you’re a healthcare provider, a patient, or a concerned family member, understanding the latest developments in sepsis management can make all the difference. Together, we can work towards a future where severe sepsis is not just a statistic but a condition that is effectively managed and, ultimately, prevented.
